Hemorrhoidal Artery Embolization
Hemorrhoidal Artery Embolization (HAE)
A Minimally Invasive Alternative to Traditional Hemorrhoid Surgery
For many adults, hemorrhoids can be painful, persistent, and disruptive to daily life. At the Vascular Institute at AMI, we offer Hemorrhoidal Artery Embolization (HAE)—an innovative, non-surgical treatment designed to relieve internal hemorrhoid symptoms with minimal discomfort.
Who Gets Hemorrhoids?
Hemorrhoids are very common—about half of all Americans will experience them at some point in their lives. In many cases, they improve on their own or with simple measures such as dietary changes, topical treatments, medications, or supplements.
However, for some people, hemorrhoids don’t go away and may cause ongoing problems like bleeding, itching, or painful bowel movements. When conservative treatments are not enough, hemorrhoids can sometimes lead to more serious complications, including:
Perianal thrombosis (a painful clot near the anus)
Incarcerated prolapsed hemorrhoids (swollen tissue that cannot be pushed back in)
Anemia from ongoing blood loss
Blood clots
Burst hemorrhoids with significant bleeding
Infection
Skin tags around the anal area
What Causes Hemorrhoids?
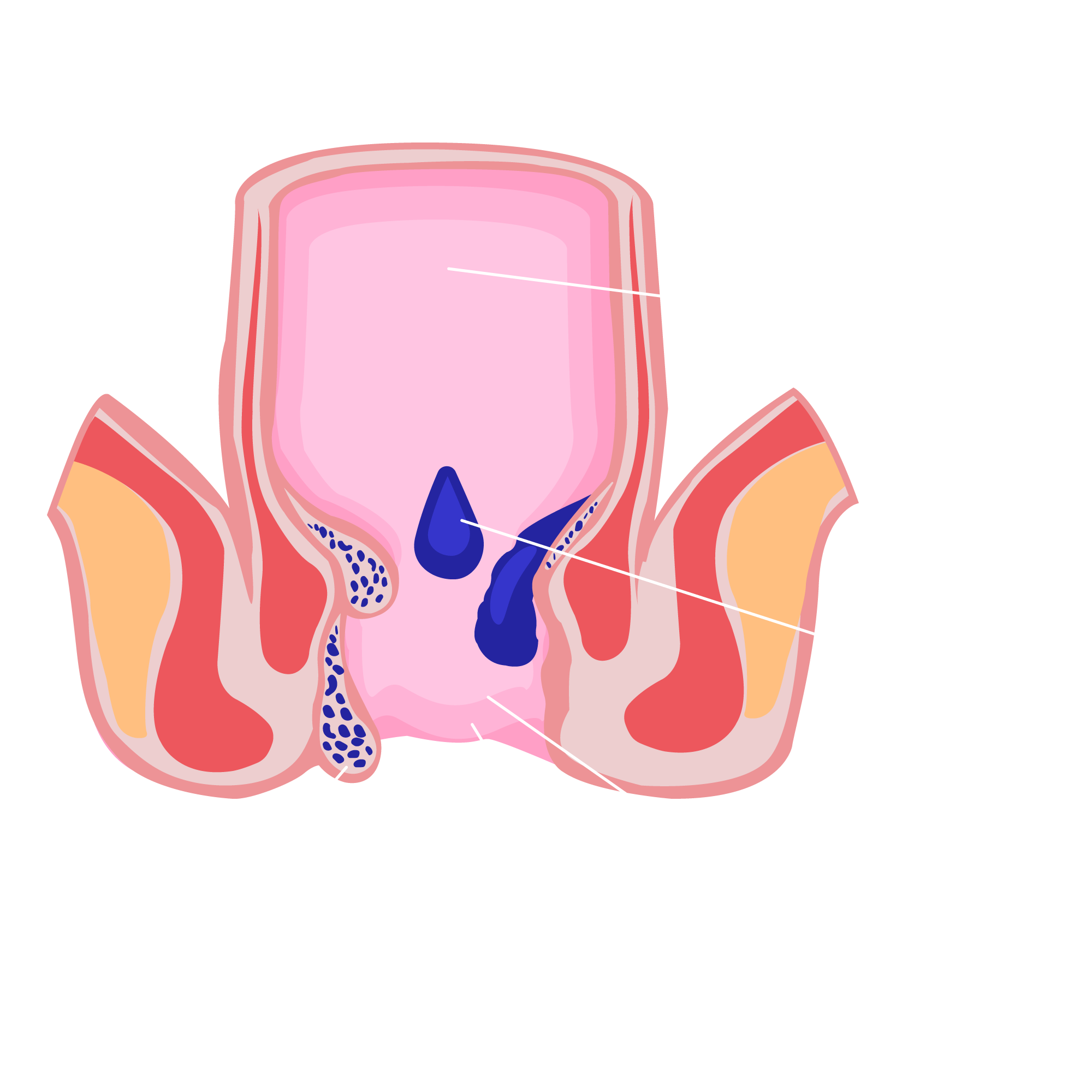
Many people misunderstand hemorrhoids. They aren’t growths but rather swollen veins in the lower rectum or under the skin around the anus—similar to varicose veins in the legs. Hemorrhoids are most common in adults between the ages of 45 and 65, and they often develop when there’s increased pressure in the rectal area.
Common factors that may contribute include:
Sitting for long periods of time
Straining during bowel movements or heavy exercise
Spinal cord injury
Chronic constipation or diarrhea
Excess weight
Pregnancy or childbirth
Family history of hemorrhoids
The good news: lifestyle changes can help lower your risk. Eating a high-fiber diet, drinking plenty of fluids, and staying physically active all support healthy digestion and may help prevent hemorrhoids.
What Are My Hemorrhoid Treatment Options?
For many people, hemorrhoids improve with simple, conservative care. This may include:
Dietary changes to add more fiber
Over-the-counter creams or ointments
Sitz baths (soaking in warm water)
Oral pain relievers such as acetaminophen (Tylenol)
If symptoms don’t improve—or if you experience severe pain, bleeding, or changes in bowel habits or stool appearance—it’s important to talk with your doctor about additional options.
-
When conservative care fails, hemorrhoidectomy may be recommended. While effective, this surgery carries risks such as infection, bleeding, bladder issues, or rectal prolapse¹ ². Recovery is also significant, often lasting 2–6 weeks.
-
This less invasive procedure places a small band around the hemorrhoid to cut off its blood supply. While commonly used, it can still be painful and may cause complications, especially for patients on blood thinners or with other medical risks.³
-
A newer, minimally invasive option, HAE is typically recommended for patients with grade 1–3 internal hemorrhoids who haven’t found relief with conservative treatments. Performed by the vascular interventional radiologists at the Vascular Institute at AMI, HAE offers effective symptom relief with less pain and quicker recovery compared to surgery.
Why Choose Hemorrhoidal Artery Embolization?
Minimally invasive and performed in an outpatient setting
HAE requires only a tiny incision—about the size of a nick in your wrist or thigh—and is performed under conscious sedation. No hospital stay is needed, and most patients return home the same day.
Faster Recovery, Less Discomfort
Unlike surgical hemorrhoid removal, which can take several weeks to recover from, HAE delivers relief with significantly less pain and downtime.
Highly Effective Results
With success rates exceeding 90%⁴, HAE effectively reduces symptoms like bleeding, pain, and swelling by gently shrinking hemorrhoidal tissue.
Lower Risk of Complications
Because this procedure avoids incisions and direct trauma to the anal region, the chances of infection, incontinence, or other complications are significantly lower compared to traditional surgery.
Is Hemorrhoidal Artery Embolization Right for You?
HAE is an excellent option for patients who:
Have internal hemorrhoids (Grade 1 to 3) that have not improved with conservative approaches.
Are seeking a less invasive alternative.
Want faster relief with minimal interruption to daily life.
What to Expect: From Consultation to Recovery
Consultation & Evaluation
Our vascular interventional radiologist will review your symptoms, medical history, and imaging to determine if Hemorrhoidal Artery Embolization (HAE) is right for you.
Procedure
On the day of your procedure, a small catheter is gently inserted—usually through the wrist or thigh—and guided to the artery supplying the hemorrhoid. Tiny coils or particles are then delivered to block the blood flow, causing the hemorrhoid to shrink and symptoms to improve.
Recovery
After the procedure, you’ will be monitored briefly and can typically go home the same day. Most patients resume normal activities within a day or two, with gradual relief from symptoms.
Talk to Your Doctor About Hemorrhoidal Artery Embolization
Hemorrhoidal Artery Embolization (HAE) is performed on an outpatient basis by the expert physicians at the Vascular Institute at AMI. Our team includes fellowship-trained vascular interventional radiologists as well as vascular surgeons, bringing together more than 100 years of combined experience. We are dedicated to providing advanced, minimally invasive treatments for a wide range of vascular conditions. If your doctor is not familiar with hemorrhoidal artery embolization, we are happy to help provide them with the information they need to make an informed recommendation.
If you think HAE may be right for you, we encourage you to schedule a consultation with our team.
Is Hemorrhoidal Artery Embolization Right for You?
You may be a candidate for HAE. Complete the form below to schedule your consultation.
Please fill out the form below so we can schedule your consultation.
-
Nearly half of all Americans will experience internal hemorrhoids at some point. These are swollen veins in the lower rectum, similar to varicose veins, and are most common in adults between 45 and 65 years of age.
-
When conservative treatments aren’t enough, hemorrhoidectomy surgery may be considered. However, recovery can be long and painful, especially since bowel movements continue during healing. Rubber band ligation is a less invasive option, but it can still cause discomfort. Hemorrhoidal artery embolization (HAE) offers a minimally invasive alternative, providing effective relief without the pain and downtime of surgery.
-
HAE is a minimally invasive, outpatient procedure that treats internal hemorrhoids through the bloodstream using imaging-guided catheters. There’s no hospital stay, reducing the risk of infection, and no large incisions or stitches—just a tiny puncture in the wrist or upper thigh, similar to a blood draw. General anesthesia is not needed.
-
Our physicians use advanced imaging to guide a tiny catheter through the bloodstream to the rectal artery. Once in place, small coils are placed in the artery feeding the hemorrhoid, causing it to shrink and relieving symptoms.
-
HAE has a success rate of over 90%, with most patients noticing significant symptom relief within 2–4 weeks.
Hemorrhoidal Artery Embolization Frequently Asked Questions
-
About 75% of patients remain free of bleeding for at least a year after HAE. If hemorrhoids return, up to 10% of patients may need a repeat procedure.
-
Hemorrhoidal Artery Embolization (HAE) is covered by most insurance plans, including Medicare. Our team can work directly with your insurance provider to confirm your coverage.
-
Complications from HAE are uncommon. In rare cases, patients may experience minor bleeding, discomfort, or infection at the catheter site. There is also a small chance (up to 10%) that hemorrhoids may return over time, but if they do, the procedure can be safely repeated.
-
If you have grade 1–3 internal hemorrhoids that haven’t improved with conservative care, HAE could offer the relief you’ve been looking for—without surgery.
-
HAE may not be suitable for patients with grade 4 prolapsed internal or external hemorrhoids, a history of colorectal surgery, severe inflammatory bowel disease, significant pelvic vascular abnormalities, allergies to contrast dye, or prior pelvic radiation therapy.
For questions or more information about the Vascular Institute at AMI,
visit vi-ami.com or call 866-356-9286.
The information contained on this website is for general information purposes only and is not intended to substitute for professional medical advice. Nothing on this site should be taken as medical advice for any individual case or situation. This information is not intended to create, and receipt or viewing does not constitute, a doctor-patient relationship. If you are suffering from a disease or ailment, you should consider seeking the counsel of a knowledgeable, licensed health care professional. Please do not use this site to disregard any medical advice, or delay seeking medical advice, because of something you read or see. We have endeavored to ensure that the information contained in this site is correct; however, we cannot guarantee it's accuracy.Hiroko Kunitake, MD, MPH and Vitaliy Poylin, MD, FACS, FASCRS2 Complications Following Anorectal Surgery Clin Colon Rectal Surg. 2016, Mar; 29(1): 14-21.Christos Simoglou et al. Milligan-Morgan Haemorrhoidectomy Complications. Hellenic Journal of Surgery 86, 68-71Andreia Albuquerque Rubber band ligation of hemorrhoids: A guide for complications. World J Gastrointest Surg. 2016 Sep 27; 8(9): 614-620Sandeep Bagla, MD et al. Outcomes of Hemorrhoidal Artery Embolization from a Multidisciplinary Outpatient Interventional Center. Journal of Vascular and Interventional Radiology.